Abstract
-
Background
In Malaysia, occupational allergic contact dermatitis (ACD) is often under-reported. This case report describes a chemical engineer who developed possible ACD, likely due to workplace allergen exposure.
-
Case presentation
He presented with a 4-month history of intensely itchy rashes on both hands, which improved during work breaks. A dermatological examination revealed lichenified, pruritic papules with well-defined borders on the palmar surfaces of both hands. A skin patch test identified reactions to five allergens, including ‘fragrance mix,’ ‘methyldibromo glutaronitrile,’ ‘clioquinol,’ ‘epoxy resin,’ and ‘textile dye mix.’ However, among these, only ‘bisphenol A diglycidyl ether,’ a component of ‘epoxy resin,’ was listed in the safety data sheet as a confirmed occupational exposure. In accordance with local regulations, this case was reported as ‘occupational dermatitis’ to the Department of Occupational Safety and Health. The patient was prescribed symptomatic topical treatments, including emollients and topical corticosteroids. Additionally, he was advised to switch to hypoallergenic products. On follow-up, his chronic inflammatory skin lesions showed improvement.
-
Conclusions
Thorough occupational history-taking and patch testing are essential for diagnosing ACD. Personalized health education and regular follow-ups, is crucial in monitoring lesion resolution and evaluating the effectiveness of preventive measures in workplace settings.
-
Keywords: Fragrance mix; Hypersensitivity; Occupational diseases; Patch tests
BACKGROUND
Contact dermatitis is an inflammatory skin condition characterized by different levels of erythema, edema, or vesiculation. It accounts for nearly 90% of all occupational skin diseases, with prevalence estimates ranging from 10% to 17%.
1,2 In the United States, the incidence rate of occupational skin diseases in 2020 was 1.8 per 10,000 workers per year.
3 Among healthcare workers, incidence rates of occupational contact dermatitis vary depending on study design. A recent systematic review found that registry-based studies reported rates between 0.6 and 6.7 cases per 10,000 person-years, whereas cohort studies showed higher rates, ranging from 15.9 to 780.0 cases per 10,000 person-years.
4
Chemical engineers are at increased risk due to their exposure to various chemicals in workplace settings, potentially leading to either irritant contact dermatitis (ICD) or allergic contact dermatitis (ACD). Notably, ICD arises when chemicals or physical agents directly exert cytotoxic effects on the skin's outermost layer (stratum corneum) at a rate exceeding the skin's ability to repair itself.
5 This leads to localized, non-immune-mediated skin reactions without the need for prior sensitization. In contrast, ACD is a delayed type of induced sensitivity triggered by cutaneous contact with exogenous agents in sensitized individuals. A skin patch test is considered the gold standard tool for diagnosing such cell-mediated type IV hypersensitivity reactions and identifying specific allergens in suspected ACD case. However, the diverse clinical presentations of occupational contact dermatitis can pose diagnostic challenges, as this skin condition often mimics other dermatological disorders such as atopic eczema, lichen planus or even cutaneous fungal infections. A thorough occupational history, combined with a detailed physical examination, appropriate diagnostic tests, and, when applicable, avoidance of suspected allergens, is essential for confirming occupational contact dermatitis.
6
Identifying geographic variations in occupational contact dermatitis enhances clinical management among Asian population.
7 However, in Malaysia, underreporting of occupational contact dermatitis (ICD or ACD) complicates epidemiological analysis, as many mild to moderate cases go unreported, leading to delays in appropriate workplace management. For example, findings from the 2023 Registry for Occupational Disease Screening in Peninsular Malaysia indicated a disparity between the prevalence of suspected occupational skin disease symptoms among Malaysian restaurant workers and the official reports, suggesting that many ICD or ACD cases go undocumented.
8
CASE PRESENTATION
This case report focuses on a chemical engineer who developed possible ACD, likely triggered by workplace allergens, highlighting the challenges of diagnosing and managing such cases in an occupational setting. Informed consent was obtained from the patient. This case report was reviewed and approved by the Institutional Review Board in Malaysia, namely the National Medical Research Registry with the identification number NMRR ID-24-03411-E0B (
https://nmrr.gov.my/research-directory/53b5678a-547a-485f-82d3-e7ae0ef2ed2a).
A Malay man in his thirties with a history of childhood bronchial asthma visited the Occupational Medicine clinic of an urban tertiary hospital, presenting with a 4-month history of an intensely itchy rash on both hands. Previously, a general practitioner had treated him for suspected hand cellulitis and superimposed fungal infection. He was prescribed a week-long course of oral cloxacillin (500 mg thrice daily) and topical antifungal cream. However, his skin condition did not improve.
Further questioning revealed that the rash, which affected mainly the third and fourth fingers, developed gradually, with symptoms easing during holidays. He had not missed work despite the rash, as it was manageable with prior pharmacological treatments. The patient was unsure whether colleagues had experienced similar skin conditions, which could be due to milder cases going unreported.
He had worked as a project engineer for 4 years, with regular exposure to workplace chemicals. He began working in the oil and gas industry in 2017 and joined a chemical engineering firm in 2020. Occasionally, he performed onsite pipeline repairs while wearing full personal protective equipment, including three layers of latex gloves, face masks, face shields, goggles, safety boots, a helmet, and a gown. The patient reported working at least eight hours per day, with less than an hour of direct exposure to industrial chemicals listed in the safety data sheet (SDS) at his workplace while performing pipeline repair. The SDS listed 11 chemicals, including ‘phenols,’ ‘polymer with formaldehyde/allyl glycidyl ether,’ ‘butane,’ ‘bisphenol A diglycidyl ether,’ ‘isophorone diamine,’ ‘methylene,’ ‘tetraethylenepentamine,’ ‘polymer with benzamine,’ ‘N-Aminoethylpiperazine,’ ‘triethylenetetramine 4%,’ and ‘ethyl alcohol.’ Intensely itchy rashes on the hands developed approximately a week after performing the specific job task of pipeline repair work, worsening on workdays and improving during breaks. He denied having direct contact with harsh cleaning products in his work environment, which could potentially compromise his skin barrier.
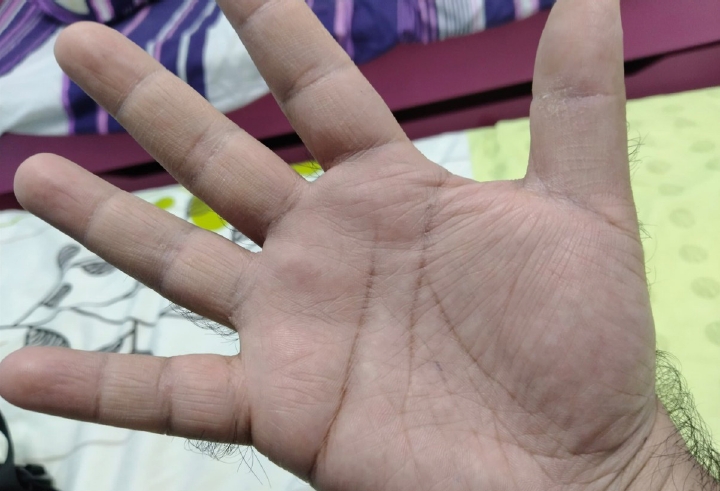
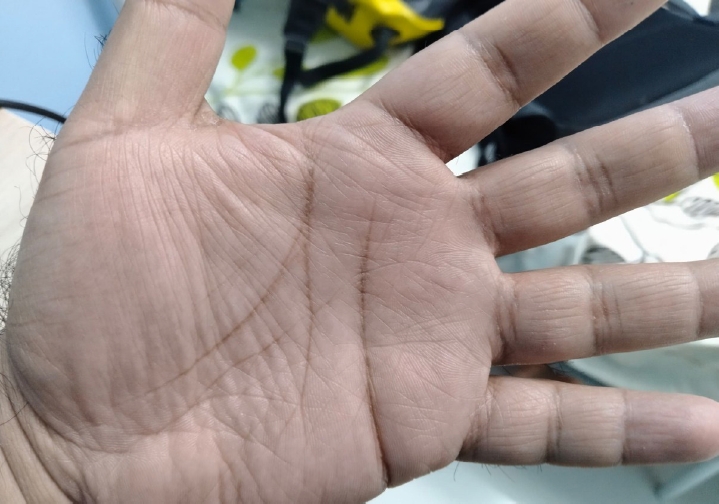
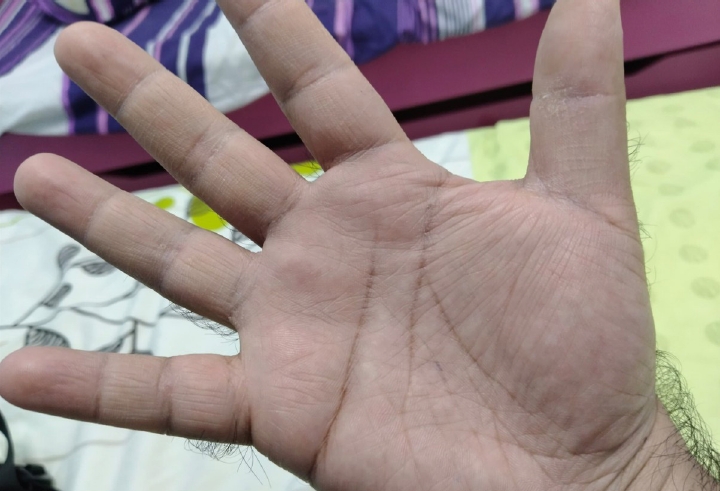
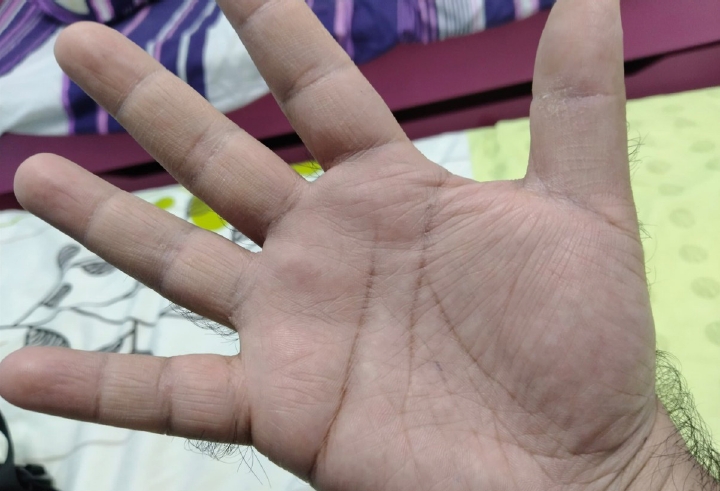
Physical examination showed pruritic papules with small (<0.5 mm) vesicles on an erythematous base around the metacarpophalangeal and interphalangeal joints of the third and fourth fingers of both hands (
Figs. 1 and
2). Lichens were noted. The lesions had well-defined borders and appeared chronic, consistent with ACD, with no signs of bacterial superinfection. A standard skin patch test with 30 antigens, as recommended in the European baseline series of contact allergens,
9 revealed reactions to ‘fragrance mix 8%’ and ‘methyldibromo glutaronitrile (MDBGN) 0.5%’ within 48 hours. At 72 hours, the test showed 1+ reactions to ‘clioquinol 5%,’ ‘epoxy resin 1%,’ and ‘fragrance mix 8%’ along with a 2+ reaction to ‘textile dye mix 6.6%.’ Notably, the patient exhibited a negative reaction to N-isopropyl-N-phenyl-4-phenylenediamine (IPPD), a chemical additive in rubber gloves that protects against oxidation of rubber and flex-cracking. The absence of a reaction suggests that IPPD is unlikely to be the causative agent for hands dermatitis in this case. Expanded skin patch testing with non-standard allergens, which might have provided more definitive insights is not done due to resource constraint.
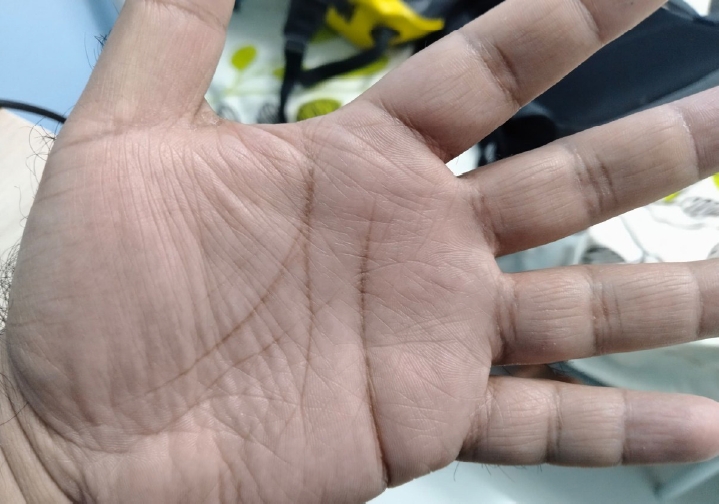
The patient was prescribed symptomatic treatments for short-term relief of pruritus namely oral cetirizine (10 mg once nightly), emollients (applied thrice daily) and topical corticosteroid namely betamethasone dipropionate 0.05% cream (applied twice daily). He was also advised to switch to hypoallergenic products and apply for compensation through the Social Security Organization. Unfortunately, a workplace assessment could not be conducted, as the patient was no longer employed by the chemical engineering firm by the time he sought treatment at the hospital. He took on a managerial role at another company, which involved minimal fieldwork. At his subsequent follow-up 6 months later, the skin lesions showed noticeable improvement with no visible papules or vesicles at the affected sites (
Figs. 3 and
4). The patient was co-managed with the Dermatologists through annual reviews for skin lesions. Notably, the lesions on his hands fully resolved after a year and have not recurred in the past 2 years.
DISCUSSION AND CONCLUSION
The occupational nature of this patient’s ACD is suspected by several key factors: the temporal relationship of symptom onset with specific job test (pipeline repair), the patient’s occupational exposure history and patch test findings. Patch testing confirmed sensitization to ‘fragrance mix,’ ‘MDBGN,’ ‘clioquinol,’ ‘epoxy resin,’ and ‘textile dye mix,’ which are commonly encountered in industrial environments. The diagnostic criteria for ACD are subsequently established based on symptom history, clinical presentation, and a positive patch test for ‘bisphenol A diglycidyl ether.’ However, distinguishing ACD from ICD based solely on history and physical examination can be challenging. Certain indicators, such as recurrent flare-ups triggered by specific job tasks and a predominantly itchy rash, may suggest ACD. In this case report, pruritus was the primary symptom, accompanied by vesicle formation.
Only one of the allergens namely ‘bisphenol A diglycidyl ether’ (which was one of the main components of ‘epoxy resin’ identified in the skin patch test) was listed in the SDS from the patient’s workplace. At least 75% of ‘epoxy resins’ used worldwide are derived from ‘bisphenol A diglycidyl ether.’
10 ‘Epoxy resin’ is widely used in industrial adhesives, coatings, and composites, which are prevalent in pipeline maintenance. Workers in construction industries are frequently exposed to epoxy-based materials, increasing their risk of developing sensitization and allergic reactions. In a cross-sectional study conducted in Finland, dermatitis was most commonly observed on the hands, forearms, or arms, affecting 69% of patch-tested patients.
11 Nitrile gloves were recommended to protect against ‘epoxy resin,’ as rubber gloves still allow resin penetration.
12 Additionally, hand protection measures, combined with the adoption of automatic production methods, have proven effective in preventing epoxy coating dermatitis.
13
This case was notified as ‘occupational dermatitis’ (item 18) to the Department of Occupational Safety and Health, as required by the Third Schedule (Regulation 7) of Occupational Safety and Health Regulations 2004. This patient was advised to delay returning to work until the skin lesions had healed, as full recovery of the epidermal barrier can take up to 2 months.
14
Workers with suspected occupational ACD should be referred by primary care providers to an Occupational Health Doctor for a comprehensive workplace assessment.
15 A detailed occupational history should be gathered at the primary care level, particularly for high-risk workers. Following a skin patch test, revisiting the occupational history may help confirm whether the identified allergens are fully or partially responsible for the skin symptoms. The mainstay treatment for ACD is to eliminate the triggering allergens; otherwise, the patient may experience chronic or recurring dermatitis.
Identifying specific allergens through skin patch tests and educating patients on how to avoid them can greatly improve the quality of life of ACD patients. In this case, the patient was advised to reduce contact with specific allergens such as ‘textile dye mix’ and ‘fragrance mix.’ ‘Textile dye mix,’ a known sensitizer, is typically used to color synthetic fabrics.
16 ‘Textile dye mix’ is frequently used in gloves and industrial fabrics, further reinforcing the likelihood of occupational exposure. The patient was advised to wear light-colored clothing made from natural fibers and to wash new clothes multiple times to remove unbound dyes. ‘Fragrance mix’ is frequently found in lubricants, cleaning solutions, and even workplace air fresheners. Furthermore, ‘fragrance mix’ is often used in workplace settings to mask unpleasant odors in products like paints and cutting fluids. The patient was advised to avoid fragranced skincare products and deodorants, a common cause of fragrance-related ACD in men.
17
The patient was also instructed to avoid products containing preservatives like ‘MDBGN.’ He was also advised to avoid using products containing ‘clioquinol’ or other quinolone compounds, as cross-sensitization may occur.
18
Despite ACD typically requires confirmation through a skin patch test, the standard testing alone may not always be sufficient to rule out a specific allergen. In this unique case, though the skin patch test yielded results for suspected chemical allergens, not all allergens were found on SDS. Many allergens capable of inducing contact dermatitis are either under-reported or absent from a conventional SDS.
19 The absence of selected patch test allergens in SDS limits Occupational Health Doctors’ ability to accurately diagnose occupational dermatitis, as SDS primarily emphasize chemical hazards but often lack detailed allergen documentation. This highlights the need for raised clinical suspicion and a comprehensive diagnostic approach when assessing ACD, as false-negatives can occur especially if the chemical allergen is rare.
For ACD diagnosis, clinicians may need to go beyond standard allergen panels and conduct specialized tests to identify less common allergens. For instance, MDBGN, previously used in industrial products but banned from cosmetics in the European Union due to its high sensitization potential, should still be tested. The prevalence of positive patch test reactions remains high in several countries, such as Turkey, likely due to past exposures or undisclosed sources.
20,21 Continued testing of MDBGN may therefore be recommended in cases of high clinical suspicion.
22 This reinforces the need for individualized patient assessment in occupational dermatology since conventional diagnostic methods are not able to capture the complete allergen spectrum.
23
Although not explicitly mentioned for ACD, underreporting of occupational illnesses can be driven by a lack of awareness, fear of job loss, and inadequate workplace health surveillance,
24 leading many workers to ignore or self-treat minor symptoms. Such an issue is further exacerbated among low-wage earners, ethnic minority workers, and those who perceive a poor psychosocial work environment.
25 Challenges in proving occupational links or limited access to specialized healthcare further contribute to underreporting.
One key limitation is the reliance on the patient’s self-reported exposure history based on SDS, which may reduce the accuracy of identifying the suspected allergen. Furthermore, the discrepancy between the patch test results and the presence of allergens in the SDS raises the possibility of patch test findings that may not be clinically relevant. Given that the SDS did not explicitly list these allergens, it is possible that the allergens were present in trace amounts or as part of chemical mixtures. This aligns with existing literature that highlights the limitations of relying solely on SDS for identifying potential occupational allergens.
26,27 Other limitations, including outdated exposure limits or missing clinical data on occupational diseases can hinder accurate risk assessment.
28
In conclusion, this case highlights the importance of identifying allergens through skin patch testing to effectively treat individuals with ACD in high-risk professions. Personalized education, follow-up and workplace adjustments are essential for long-term recovery and reducing the impact of ACD.
Abbreviations
allergic contact dermatitis
irritant contact dermatitis
N-isopropyl-N-phenyl-4-phenylenediamine
methyldibromo glutaronitrile
NOTES
-
Competing interests
The authors declare that they have no competing interests.
-
Author contributions
Conceptualization: Yap JF. Data curation: Yap JF. Formal analysis: Yap JF. Investigation: Supramanian RK, Lim YC. Methodology: Yap JF. Writing - original draft: Yap JF. Writing - review & editing: Supramanian RK, Lim YC, Wan KS, Mohd Yusoff MF.
-
Acknowledgments
We sincerely thank Dr Faiz Baharudin and Dr Venna Magarita from Department of Public Health, Universiti Malaya Medical Centre for their collaboration in managing this case. We would also like to thank the Director General of Health Malaysia for his permission to publish this article.
Fig. 1.Left hand’s skin condition before treatment.

Fig. 2.Right hand’s skin condition before treatment.

Fig. 3.Left hand’s skin condition after treatment.
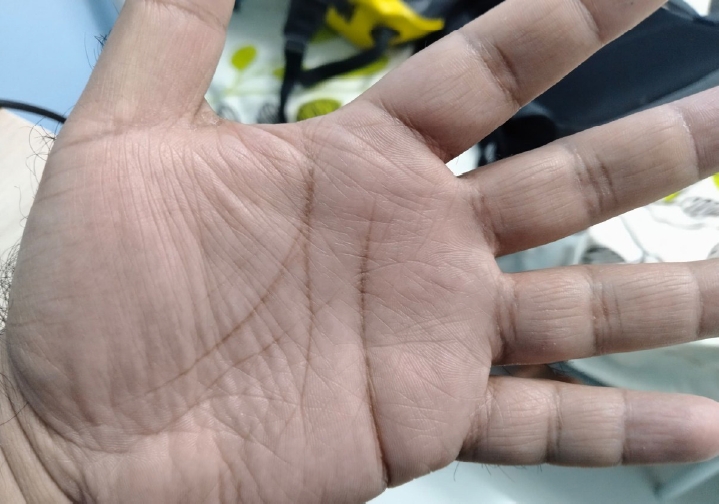
Fig. 4.Right hand’s skin condition after treatment.
REFERENCES
- 1. Lee J, Lin R, Maderal A. Update on occupational dermatitis: reviewing toxic substances from OSHA standards. Int J Dermatol 2025;64(1):72–8.ArticlePubMedPMC
- 2. Milam EC, Nassau S, Banta E, Fonacier L, Cohen DE. Occupational contact dermatitis: an update. J Allergy Clin Immunol Pract 2020;8(10):3283–93.ArticlePubMed
- 3. Karagounis TK, Cohen DE. Occupational hand dermatitis. Curr Allergy Asthma Rep 2023;23(4):201–12.ArticlePubMedPMCPDF
- 4. Larese Filon F, Pesce M, Paulo MS, Loney T, Modenese A, John SM, et al. Incidence of occupational contact dermatitis in healthcare workers: a systematic review. J Eur Acad Dermatol Venereol 2021;35(6):1285–9.ArticlePubMedPMCPDF
- 5. Kezic S, Visser MJ, Verberk MM. Individual susceptibility to occupational contact dermatitis. Ind Health 2009;47(5):469–78.ArticlePubMed
- 6. Pesque D, Aerts O, Bizjak M, Goncalo M, Dugonik A, Simon D, et al. Differential diagnosis of contact dermatitis: a practical-approach review by the EADV Task Force on contact dermatitis. J Eur Acad Dermatol Venereol 2024;38(9):1704–22.ArticlePubMed
- 7. Bhatia R, Sharma VK. Occupational dermatoses: an Asian perspective. Indian J Dermatol Venereol Leprol 2017;83(5):525–35.ArticlePubMed
- 8. Ahmad Fuad MH, Samsudin EZ, Yasin SM, Ismail N, Mohamad M, Muzaini K, et al. Prevalence and associated factors of suspected occupational skin diseases among restaurant workers in peninsular Malaysia: secondary data analysis of Registry for Occupational Disease Screening (RODS). BMJ Open 2024;14(8):e079877.ArticlePubMedPMC
- 9. Johansen JD, Aalto-Korte K, Agner T, Andersen KE, Bircher A, Bruze M, et al. European Society of Contact Dermatitis guideline for diagnostic patch testing: recommendations on best practice. Contact Dermatitis 2015;73(4):195–221.ArticlePubMed
- 10. Karlsson I, Ponting DJ, Ortega MA, Niklasson IB, Ndreu L, Steen EJL, et al. Nature-derived epoxy resin monomers with reduced sensitizing capacity horizontal line isosorbide-based bis-epoxides. Chem Res Toxicol 2023;36(2):281–90.ArticlePubMedPMCPDF
- 11. Aalto-Korte K, Pesonen M, Suuronen K. Occupational allergic contact dermatitis caused by epoxy chemicals: occupations, sensitizing products, and diagnosis. Contact Dermatitis 2015;73(6):336–42.ArticlePubMedPDF
- 12. Henriks-Eckerman ML, Makela EA, Suuronen K. Testing penetration of epoxy resin and diamine hardeners through protective glove and clothing materials. Ann Occup Hyg 2015;59(8):1034–43.ArticlePubMed
- 13. Yokota K, Johyama Y, Yamaguchi K. Occupational dermatoses from one-component epoxy coatings containing a modified polyamine hardener. Ind Health 2000;38(3):269–72.ArticlePubMed
- 14. Segre JA. Epidermal barrier formation and recovery in skin disorders. J Clin Invest 2006;116(5):1150–8.ArticlePubMedPMC
- 15. Awaluddin SM, Mahjom M, Lim KK, Shawaluddin NS, Tuan Lah TM. Occupational disease and injury in Malaysia: a thematic review of literature from 2016 to 2021. J Environ Public Health 2023;2023:1798434.ArticlePubMedPMCPDF
- 16. Malinauskiene L, Bruze M, Ryberg K, Zimerson E, Isaksson M. Contact allergy from disperse dyes in textiles: a review. Contact Dermatitis 2013;68(2):65–75.ArticlePubMed
- 17. Heisterberg MV, Menne T, Andersen KE, Avnstorp C, Kristensen B, Kristensen O, et al. Deodorants are the leading cause of allergic contact dermatitis to fragrance ingredients. Contact Dermatitis 2011;64(5):258–64.ArticlePubMed
- 18. Kreft B, Wohlrab J. Contact allergies to topical antibiotic applications. Allergol Select 2022;6:18–26.ArticlePubMedPMC
- 19. Brans R, Skudlik C. Patch testing in occupational dermatology: practical aspects in relation to the conditions in Germany. Allergol Select 2024;8:82–9.ArticlePubMedPMC
- 20. Ozkaya E, Mangir O. High prevalence but no current clinical relevance of methyldibromo glutaronitrile since its ban in Turkey in 2015. Contact Dermatitis 2024;91(4):306–16.ArticlePubMed
- 21. Surgun E, Boyvat A. Increased rates of contact allergy to selected preservatives in patients with allergic contact dermatitis in Turkey. Contact Dermatitis 2024;90(2):110–5.ArticlePubMed
- 22. Liden C, White IR. Comment on MDBGN/DBDCB, the European baseline series, and EU legislation. Contact Dermatitis 2021;85(5):607–10.ArticlePubMedPDF
- 23. Houle MC, Holness DL, DeKoven J. Occupational contact dermatitis: an individualized approach to the worker with dermatitis. Curr Dermatol Rep 2021;10(4):182–91.ArticlePubMedPMCPDF
- 24. Kreshpaj B, Bodin T, Wegman DH, Matilla-Santander N, Burstrom B, Kjellberg K, et al. Under-reporting of non-fatal occupational injuries among precarious and non-precarious workers in Sweden. Occup Environ Med 2022;79(1):3–9.ArticlePubMedPMC
- 25. Kyung M, Lee SJ, Dancu C, Hong O. Underreporting of workers' injuries or illnesses and contributing factors: a systematic review. BMC Public Health 2023;23(1):558.ArticlePubMedPMCPDF
- 26. Clynick M, Holness DL. New causes of occupational allergic contact dermatitis. Curr Opin Allergy Clin Immunol 2024;24(2):51–7.ArticlePubMed
- 27. Lampel HP, Powell HB. Occupational and hand dermatitis: a practical approach. Clin Rev Allergy Immunol 2019;56(1):60–71.ArticlePubMedPDF
- 28. Friis UF, Menne T, Flyvholm MA, Bonde JP, Johansen JD. Difficulties in using material safety data sheets to analyse occupational exposures to contact allergens. Contact Dermatitis 2015;72(3):147–53.ArticlePubMed
 , Kim Sui Wan1
, Kim Sui Wan1 , Muhammad Fadhli Mohd Yusoff1
, Muhammad Fadhli Mohd Yusoff1 , Yin Cheng Lim2,3
, Yin Cheng Lim2,3 , Rama Krishna Supramanian2,3,*
, Rama Krishna Supramanian2,3,*



 KSOEM
KSOEM



 Cite
Cite

