Abstract
-
Background
Lead poisoning is a serious public health issue that can arise from various sources, including nonoccupational exposure. This can make it challenging to manage, as lead poisoning can arise from unexpected sources. This case study examined lead poisoning in a 52-year-old man linked to hobbyist activities involving lead pellets, highlighting the diagnostic and therapeutic challenges associated with this uncommon source of exposure.
-
Case presentation
A 52-year-old man with a history of sports fishing presented with confusion, balance disorders, and memory loss. The initial medical evaluation revealed anemia and elevated lead levels. Further investigations, including imaging and blood tests, confirmed the presence of ingested lead pellets. The patient underwent chelation therapy, which led to a reduction in blood lead levels and improvement in symptoms. Follow-up over 46 months showed a gradual decrease in lead levels and partial recovery of cognitive function, although a few lead-related effects persisted.
-
Conclusions
This case underscores the need for awareness of non-traditional sources of lead exposure, such as hobbyist activities. Effective diagnosis and treatment, including chelation therapy, can significantly alleviate the effects of lead poisoning. Ongoing monitoring is essential to manage long-term health outcomes related to chronic lead exposure.
-
Keywords: Lead poisoning; Environmental exposure; Cognition disorders; Chronic disease; Monitoring, physiologic; Hobbies
BACKGROUND
Lead has been used in various contexts throughout history in both its organic and inorganic forms.
1,2 Exposure to lead can occur primarily through ingestion or inhalation; however, cases of exposure through the skin and during gestation have also been documented.
3,4 In adults, exposure primarily occurs in work environments where lead vapor and dust are inhaled.
5,6
Nonoccupational exposure, primarily from domestic sources, is more common in children, primarily because of their tendency to put various objects in their mouths; items that may contain lead include paints, water, soil, food, toys, cosmetics, natural remedies, and alternative medicines.
7
Lead poisoning, which is primarily caused by absorption through the respiratory and gastrointestinal tracts, can lead to the distribution of the metal to various organs, including the nervous system.
8,9 Clinically, it presents with nonspecific symptoms, such as abdominal pain, constipation, and irritability, along with severe neurological symptoms, such as seizures and coma. The nervous system is particularly susceptible, especially with prolonged exposure potentially affecting memory and attention.
9
Managing lead poisoning can at times be challenging, as lead poisoning can stem from unexpected sources, such as hunting bullets, although this possibility may seem more theoretical than practical.
10
The present case involved a 52-year-old man in good health who was admitted to the hospital because of confusion, balance disorders, and amnesia. He also reported asthenia, muscle weakness, retrosternal pyrosis, and abdominal pain, leading to a diagnosis of lead poisoning.
CASE PRESENTATION
Clinical course and diagnosis of lead poisoning related to recreational fishing
A previously healthy 52-year-old man was admitted in July 2020 to a peripheral hospital owing to symptoms including confusion, balance disorders, amnesia, asthenia, muscle weakness, retrosternal pyrosis, and lower abdominal pain over the previous 3 months. During medical history intake, it was noted that the man worked as an employee at a fish processing plant and practiced sport fishing as a hobby.
Laboratory tests conducted during admission revealed anemia (hemoglobin: 7.5 g/dL), severe hyponatremia (Na
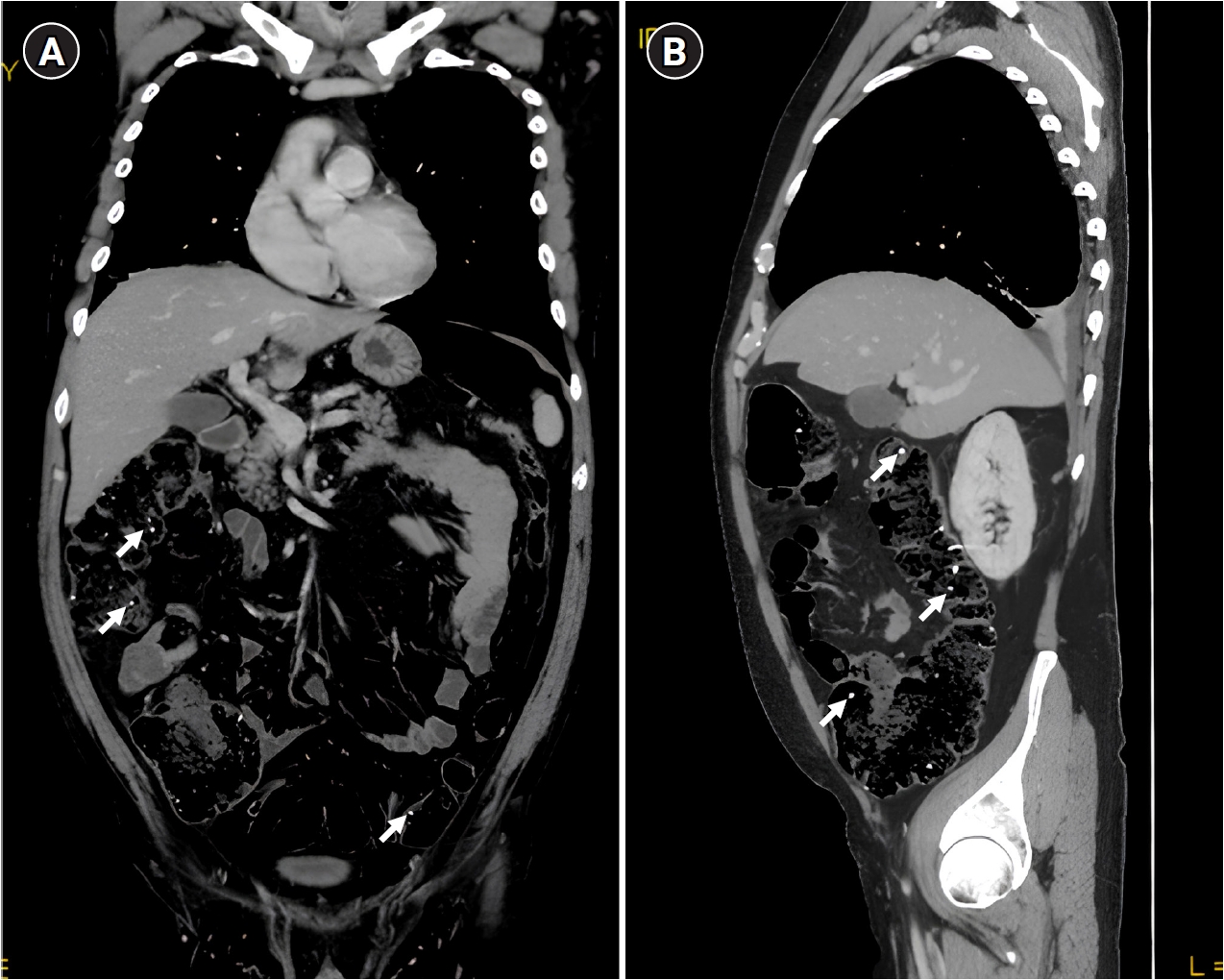
+: 116 mEq/L), and increased inflammation markers (C-reactive protein: 4.57 mg/dL). The patient received empirical antibiotic therapy and a hypertonic solution. Owing to the suspicion of myeloproliferative disease, colonoscopy, gastroscopy, and a total body computed tomography (CT) scan were performed, which revealed hyperdense punctiform images suggestive of ingestion (
Fig. 1).
Anisocytosis and anisochromia consistent with lead anemia were observed in a peripheral venous blood smear. The patient was initially discharged with a diagnosis of “anemia, leukocytosis, and acute hepatitis due to lead accumulation in blood.”
Subsequently, the first peripheral venous blood sample tested post-discharge revealed elevated blood lead (Pb-B) levels of 54.6 µg/dL (reference range: 0–16 µg/dL). Further evaluation at the toxicology clinic revealed a Pb-B concentration of 93 µg/dL (reference range: 0–16 µg/dL), urinary lead (Pb-U) at 111.2 µg/g (reference range: 1.0–18.0 µg/g), porphobilinogen (PBG) at 0.94 mg/g (reference range: 0.0–2.0 mg/g), delta-aminolevulinic acid (dALA) at 23.5 mg/g (reference range: <6.0 mg/g), and zinc-protoporphyrin IX (ZPP) at 146.3 µg/dL (reference range: <40 µg/dL).
Upon admission to the Occupational Medicine Clinic in October of the same year, the patient exhibited normochromic normocytic anemia, Pb-B of 66 µg/dL, ZPP of 183.9 µg/dL, Pb-U of 1,166.0 µg/g, and dALA of 2 mg/g. During anamnesis, the patient reported a habitual practice of biting lead sinkers before attaching them to the fishing line. Lead sinkers are small, dense weights made primarily of lead (typically 95%–100% pure), used in recreational fishing to stabilize fishing lines and improve casting accuracy; these sinkers are commonly attached to fishing lines and are often manually adjusted by anglers, sometimes by biting them to secure their placement. This behavior intensified during the March–April 2020 lockdown, significantly increasing the likelihood of ingestion. A CT scan performed at admission identified hyperdense punctiform images in the gastrointestinal tract, consistent with metallic foreign bodies resembling lead pellets (
Fig. 1). Laboratory findings further supported significant lead exposure, with markedly elevated Pb-B and Pb-U levels. Additionally, peripheral blood smear analysis demonstrated anisocytosis and anisochromia, both characteristic of lead-induced anemia. Notably, a thorough toxicological evaluation ruled out alternative occupational or environmental sources of lead exposure, reinforcing the conclusion that the ingestion of fishing pellets was the primary route of intoxication.
During hospitalization, various instrumental examinations, including cardiac Doppler ultrasonography, electroencephalography, electromyography, and encephalic magnetic resonance imaging, were conducted, all of which yielded normal results. Hearing function assessment by tonal audiometry was also performed, which showed asymmetric hearing loss. The possibility of an occupational origin of the hearing loss was rejected, as during all his work activity the patient had never been exposed to noise risk. Chelation therapy with EDTA was administered for 4 days, leading to reduced lead levels upon discharge (Pb-B: 39 µg/dL [normal value: 1–16], Pb-U: 133 µg/g, and ZPP: 185.9 µg/dL).
Neuropsychological assessments were also performed, including screening of cognitive function (Mini-Mental State Examination test, Hasegawa’s Dementia Scale [HDS], and clock drawing test), executive function (Frontal Assessment Battery test), attention (Trail Making Test [TMT]-A, TMT-B, TMT B-A, and digit symbol substitution test), memory (digit span forward, Digit Span Backward, Rey’s 15 Words and Anna Pesenti's Short Story), visuoconstructive skills (copy of drawings, copy of drawings with programming elements), logical-perceptual skills (Raven '47 Progressive Matrices) and language (phonemic verbal fluency and semantic verbal fluency). In all assessments, the impairment highlighted was selective deficits in verbal memory, with an improving trajectory at the 1-year control assessments.
Specifically, the trend of mnemonic test results was as follows: digit span forward 4.6 (statistical reference prediction error [PE]=2) to 4.6 (statistical reference PE=2), digit span backward 3.5 (statistical reference PE=1) to digit span backward 4.5 (statistical reference PE=4), Rey’s 15-word test immediate reenactment 29.7/75 (statistical reference PE=1) to 36.7/75 (statistical reference PE=3), deferred reenactment 2.5/15 (statistical reference PE=0) to 7.5/15 (statistical reference PE=3), recognition real 11, false 1 to real 12 false 0, short story 7.5/28 (statistical reference PE=0) to 12.5/28 (statistical reference PE=3).
Follow-up examinations at 2 months, 3 months, 6 months, and 1 year revealed a gradual reduction in lead levels over time (
Table 1).
The investigations conducted 4 years later revealed the following: blood and urine tests showed mean corpuscular hemoglobin concentration 31.9 g/dL, total protein 6.5 g/dL, and ZPP 16 µg/dL with Pb-B and Pb-U excretion levels were high, Pb-B levels were elevated, whereas the Pb-U levels had normalized. And 24-hour urine analysis for PBG and dALA levels showed quantitative PBG 0.22 mg/L, quantitative PBG 0.15 mg/g creatinine (normal range: 0.00–2.00 mg/g), and dALA 1.3 mg/g creatinine (normal range: <6.0 mg/g) (
Table 1).
The clinical condition of the patient remained stable during follow-up, which was conducted 4 years after exposure. During the hospital stay, the patient underwent a series of laboratory and instrumental tests to reassess their clinical condition after chronic lead poisoning. No cerebral or cardiac abnormalities were detected; however, hearing impairment of unclear significance was confirmed. Moreover, reassessment of cognitive status confirmed memory and behavioral alterations previously identified during the previous evaluation; instead, the mini-mental state examination and HDS, equal to 26.31/30 (cut-off >23.80) and HDS 11/16 (cut-off >9) respectively, increased at the last checkup to 29/30 and 16/16.
As this is a case report, written informed consent was obtained from the patient for the publication of clinical data and any accompanying images. Ethical approval from the local ethics committee was not required, as the report does not involve a clinical trial or systematic research involving human subjects.
DISCUSSION AND CONCLUSION
The clinical scenario outlined here is noteworthy because of its unique etiology. Lead poisoning originating from nonoccupational sources is not rare, although it is more commonly observed in pediatric cases and often associated with the pica phenomenon, which are linked to economic, social, and/or environmental factors associated with reduced socioeconomic circumstances, highlighting poverty as a contributing factor.
11-13
However, the scenario presented did not clearly fit either classification. Instead, it emphasizes a predominantly nonoccupational source of lead contamination, particularly from hobbyist activities, one of the least common sources.
10
From the reconstruction performed by the clinical staff, it was determined that the poisoning originated from lead pellets used for sports fishing.
This case aligns with broader research highlighting the environmental and public health concerns of lead exposure from recreational activities. Studies such as those conducted by Guitart et al.
14 emphasize the extensive dispersion of lead from ammunition and fishing weights, with well-documented toxic effects on avian species. Waterfowl and birds of prey are particularly vulnerable, as they may ingest lead pellets mistaken for grit or accumulate lead through the food chain. Our case provides direct clinical evidence of lead poisoning in a human patient following a similar exposure pathway, underscoring the need for increased regulation of lead-based fishing gear.
Furthermore, these pellets were often bitten with the teeth before being attached to the fishing line and accidentally ingested on multiple occasions, as evidenced by the CT scan performed upon admission.
Instances of unintentional poisoning in adults primarily arise from hunting activities (as a result of consuming game animals such as fish, which may contain lead residues) or occur within domestic environments. Another aspect worth considering is the clinical manifestations.
15 Lead poisoning commonly initially presents with gastrointestinal symptoms, which can sometimes lead to misdiagnosis because it is not often considered among the primary differential diagnoses for acute abdominal conditions.
16,17
In this particular case, the primary concern was cognitive impairments. What distinguishes these impairments is that they occurred in an adult subject who did not experience the detrimental effects of lead on the nervous system (including the central nervous system) during development, unlike pediatric patients. Notably, the greatest risk during childhood is the potential for irreversible disability and cognitive impairment; in severe cases, it may even lead to seizures, coma, or death.
18
In the present case, the subject affected by neurocognitive deficits was a 52-year-old adult, illustrating that lead has neurocognitive effects even in the nervous system of adults. Furthermore, no alternative explanation for these effects other than lead poisoning could be found.
In addition, the patient in this case demonstrated a partial reversal of amnestic deficits, which coincided with a partial reduction in Pb-B values.
Moreover, the results of the follow-up conducted 4 years after the initial visit (46 months) are noteworthy. Most notable were the findings regarding Pb-B levels (which remained elevated despite exposure having ceased years ago), auditory impairments, and the persistence of memory deficits. The elevated Pb-B levels years after exposure may be attributed to the release of metal from the bone matrix, where it is stored.
19
Although these latter issues seem specific and warrant further investigation through large-scale studies, this observation seems to support the idea that chronic lead poisoning has long-term cognitive and neurosensory effects and highlights the role of bone deposits in sustaining increased Pb-B levels long after the cessation of exposure.
Limits
As a single-case report, its findings lack generalizability and do not allow for definitive conclusions regarding the prevalence or long-term consequences of chronic lead exposure in similar contexts. While the study documents cognitive improvements over time, it cannot establish a direct causal relationship between lead exposure and the observed neurocognitive effects, as other environmental factors or individual predispositions may have influenced the clinical outcome. Furthermore, the absence of advanced neuroimaging assessments or specific biomarkers limits a comprehensive understanding of the neurotoxic mechanisms underlying chronic lead poisoning. Future studies with larger sample sizes and extended follow-up periods are warranted to provide more robust data on the long-term impact of lead exposure.
Environmental impact of lead exposure from fishing activities in the country where the case occurred
In Italy, the use of lead sinkers in recreational fishing is regulated to mitigate environmental pollution and reduce lead poisoning risks. These regulations align with European Union directives on hazardous substances and environmental protection.
20 The Italian Legislative Decree No. 152/2006 (Environmental Code) establishes principles for controlling water pollution, including contamination from heavy metals such as lead.
21 Additionally, the Ministerial Decree of 17 October 2008 introduced specific restrictions on hazardous substances in fishing activities, particularly in ecologically sensitive areas.
Beyond national regulations, several regional and local authorities have imposed additional limitations on the use and sale of lead sinkers, particularly in protected marine areas, national parks, and nature reserves. In some regions, recreational anglers are required to use non-toxic alternatives such as tungsten, steel, or ceramic sinkers to prevent lead contamination in aquatic ecosystems.
22
From a preventive perspective, awareness campaigns led by governmental agencies and environmental organizations aim to educate the public on lead exposure risks and promote environmentally friendly fishing practices. Some fishing associations have also adopted voluntary lead-reduction programs, encouraging members to transition to non-toxic fishing gear. Additionally, discussions at the national and European Union levels continue regarding the progressive phase-out of lead-based fishing equipment, reflecting a broader commitment to environmental and public health protection.
23
This case underscores the critical need for greater awareness of lead exposure risks stemming from recreational activities, which are often underestimated compared to occupational or environmental exposures. Preventing similar incidents requires targeted interventions, including the adoption of non-toxic alternatives to lead fishing sinkers, public education campaigns for anglers and hunters on the dangers of accidental lead ingestion, and proactive health screenings for individuals engaged in high-risk activities. Additionally, long-term monitoring of lead-exposed patients could enhance our understanding of the trajectory of neurocognitive effects and help identify more effective therapeutic approaches. Regulatory measures restricting the use of lead in recreational materials could represent a crucial step in mitigating the risk of chronic exposure and safeguarding public health.
Lead poisoning poses significant health risks and can stem from various sources, including nonoccupational exposures such as hobbyist activities. This case emphasizes the need to increase awareness of unconventional sources of lead contamination.
The clinical and toxicological findings reinforce the urgency of regulatory measures restricting the use of lead in recreational fishing and hunting gear.
Given the well-documented environmental and human health risks associated with lead exposure, greater efforts are needed to promote non-toxic alternatives, improve public education on exposure pathways, and implement routine screening for individuals engaged in high-risk activities. Our findings further support existing policies aimed at reducing lead-related hazards and call for continued surveillance to prevent similar cases of chronic lead intoxication.
Abbreviations
delta-aminolevulinic acid
Hasegawa’s Dementia Scale
NOTES
-
Competing interests
The authors declare that they have no competing interests.
-
Author contributions
Conceptualization: Pucci C, Tomassini L, Deini A, Gambelunghe A. Data curation: Tomassini L, Zampolini M. Formal analysis: Zampolini M, Gambelunghe C. Investigation: Gambelunghe C. Supervision: Gambelunghe A. Software and visualization: Lillacci D. Discussion and interpretation: Murgia N. Writing - original draft: Pucci C, Deini A. Writing - review & editing: dell’Omo M, Gambelunghe A.
Fig. 1.Radiopaque foreign bodies identified within the bowel on computed tomography imaging. (A) Coronal plane. (B) Sagittal plane.

Table 1.Progression of Pb values during the clinical course, post-therapy, and throughout the conducted follow-up assessments
|
Date |
Pb-B (n.v. 1.0–16.0 μg/dL) |
Pb-U (n.v. 1.0–18.0 μg/g.creat) |
PBG (n.v. 0–2 mg/g.creat) |
dALA (n.v. <6.0 mg/g.creat) |
ZPP (n.v. 0–40.0 μg/dL) |
|
August 5, 2020 (after discarge) |
54.6 |
- |
- |
- |
- |
|
September 9, 2020 (cessation of exposure) |
93 |
111.2 |
0.94 |
23.5 |
146.3 |
|
October 22, 2020 (recovery admission) |
66 |
1,166.0 |
- |
2 |
183.9 |
|
October 27, 2020 (4 days after EDTA therapy) |
39 |
133 |
- |
- |
185.9 |
|
December 4, 2020 (2 months follow-up) |
56 |
76.7 |
0.63 |
1.1 |
133.2 |
|
January 26, 2021 (3 months follow-up) |
38 |
20.7 |
2.2 |
2.2 |
56.6 |
|
April 8, 2021 (6 months follow-up) |
28 |
26.1 |
- |
3.7 |
26.4 |
|
September 30, 2021 (12 months follow-up) |
28 |
18 |
- |
3 |
21 |
|
March 22, 2022 (18 months follow-up) |
11.97 |
56.6 |
- |
5.4 |
- |
|
July 17, 2024 (46 months follow-up) |
22.0 |
7.0 |
0.15 |
1.3 |
160 |
REFERENCES
- 1. Waldron HA. Lead poisoning in the ancient world. Med Hist 1973;17(4):391–9.ArticlePubMedPMC
- 2. Acharya S. Lead between the lines. Nat Chem 2013;5(10):894.ArticlePubMedPDF
- 3. Rastogi SC, Clausen J. Absorption of lead through the skin. Toxicology 1976;6(3):371–6.ArticlePubMed
- 4. Santana AB, Spelta LE, Sobalvarro JVM, Podesta M, Garcia RC, Dos Reis TM, et al. Gestational lead exposure and its effects on fetal/infant development: a systematic review. Reprod Toxicol 2023;117:108342.ArticlePubMed
- 5. Tong S, von Schirnding YE, Prapamontol T. Environmental lead exposure: a public health problem of global dimensions. Bull World Health Organ 2000;78(9):1068–77.PubMedPMC
- 6. Juberg DR, Kleiman CF, Kwon SC. Position paper of the American Council on Science and Health: lead and human health. Ecotoxicol Environ Saf 1997;38(3):162–80.ArticlePubMed
- 7. Dapul H, Laraque D. Lead poisoning in children. Adv Pediatr 2014;61(1):313–33.ArticlePubMed
- 8. Hosseini MS, Salimi A, Phillips S, Zamani N, Hassanian-Moghaddam H. Adult lead poisoning caused by contaminated opium: a two-year longitudinal follow-up study. Ann Glob Health 2021;87(1):89.ArticlePubMedPMC
- 9. Wani AL, Ara A, Usmani JA. Lead toxicity: a review. Interdiscip Toxicol 2015;8(2):55–64.ArticlePubMedPMC
- 10. Leontowich AF, Panahifar A, Ostrowski R. Fragmentation of hunting bullets observed with synchrotron radiation: lighting up the source of a lesser-known lead exposure pathway. PLoS One 2022;17(8):e0271987.ArticlePubMedPMC
- 11. Leung AK, Hon KL. Pica: a common condition that is commonly missed - an update review. Curr Pediatr Rev 2019;15(3):164–9.ArticlePubMed
- 12. Mohammadyan M, Moosazadeh M, Borji A, Khanjani N, Rahimi Moghadam S. Investigation of occupational exposure to lead and its relation with blood lead levels in electrical solderers. Environ Monit Assess 2019;191(3):126.ArticlePubMedPDF
- 13. Kim MA, Williams KA. Lead levels in landfill areas and childhood exposure: an integrative review. Public Health Nurs 2017;34(1):87–97.ArticlePubMedPDF
- 14. Guitart R, Sachana M, Caloni F, Croubels S, Vandenbroucke V, Berny P. Animal poisoning in Europe. Part 3: Wildlife. Vet J 2010;183(3):260–5.ArticlePubMed
- 15. Anderson WL, Havera SP, Zercher BW. Ingestion of lead and nontoxic shotgun pellets by ducks in the Mississippi Flyway. J Wildl Manag 2000;64(3):848–57.Article
- 16. Safaee M, Malekzadeh M, Motamedi N, Sayadishahraki M, Eizadi-Mood N. Gastrointestinal manifestations of lead poisoning: a brief report. Iran J Med Sci 2023;48(6):600–5.ArticlePubMedPMC
- 17. Kaneko M, Kazatani T, Shikata H. Occupational lead poisoning in a patient with acute abdomen and normocytic anemia. Intern Med 2020;59(12):1565–70.ArticlePubMedPMC
- 18. Naranjo VI, Hendricks M, Jones KS. Lead toxicity in children: an unremitting public health problem. Pediatr Neurol 2020;113:51–5.ArticlePubMed
- 19. Rabinowitz MB. Toxicokinetics of bone lead. Environ Health Perspect 1991;91:33–7.ArticlePubMedPMC
- 20. European Environment Agency. Progress in regulating lead (signal). https://www.eea.europa.eu/en/european-zero-pollution-dashboards/indicators/progress-in-regulating-lead-signal. Updated 2024. Accessed March 12, 2025
- 21. Legislative Decree No. 152/2006 approving the Code on the Environment. FAOLEX database. https://www.fao.org/faolex/results/details/en/c/LEX-FAOC064213/. Updated 2025. Accessed March 12, 2025
- 22. Law No. 394 of December 6, 1991. Framework Law on Protected Areas. Gazzetta Ufficiale della Repubblica Italiana. Serie Generale. December 13, 1991. No. 292, Ordinary Supplement No. 83.
- 23. Wood KA, Newth JL. Swans and lead fishing weights: a systematic review of deposition, impacts and regulations in Europe. Wildfowl 2024;7:27–56.
 , Luca Tomassini2
, Luca Tomassini2 , Marco dell’Omo1
, Marco dell’Omo1 , Alessandra Deini1
, Alessandra Deini1 , Daniele Lillacci1
, Daniele Lillacci1 , Cristiana Gambelunghe3
, Cristiana Gambelunghe3 , Mauro Zampolini4
, Mauro Zampolini4 , Nicola Murgia5
, Nicola Murgia5 , Angela Gambelunghe1,*
, Angela Gambelunghe1,*







 KSOEM
KSOEM

 Cite
Cite

